Glaucoma Surgery is incisional surgery performed on the eye, in an operating room, using an operating microscope. Glaucoma surgery can be performed by itself, or sometimes combined with cataract surgery. There are many different types of glaucoma surgery.
All glaucoma surgeries share in common the purpose of increasing the drainage of aqueous humor fluid from the eye in order to lower the pressure inside the eye.
Glaucoma surgery procedures can be minimally invasive, taking just minutes to perform with rapid recovery, or can be more complex procedures that take longer to perform with longer recovery times. The surgeries are almost always performed as same day, outpatient surgery.
The type of surgery that is best suited for a patient depends on many factors including the type of glaucoma, how high the pressure is, how low the pressure needs to be, how quickly the pressure needs to be lowered, the stage of the glaucoma, and the overall health of the eye.
Minimally Invasive Glaucoma Surgery (MIGS) refers to a group of procedures that are performed relatively quickly with little manipulation to the eye, usually under topical (eye drop) anesthesia, using small incisions and no sutures. The goal of a MIGS procedure is to provide rapid recovery while minimizing the risks associated with conventional glaucoma surgery.
As a general rule, the less invasive a procedure, the less likely it is to achieve a significant change in the eye pressure or continue to function long-term. Therefore, there is a trade-off between the degree of safety and the effectiveness of the procedure.
Some MIGS procedures (such as the iStent and Hydrus) are reserved for more mild types of glaucoma that are being treated at an early stage. Other MIGS procedures (such as the XEN stent) can be performed on more advanced glaucomas.
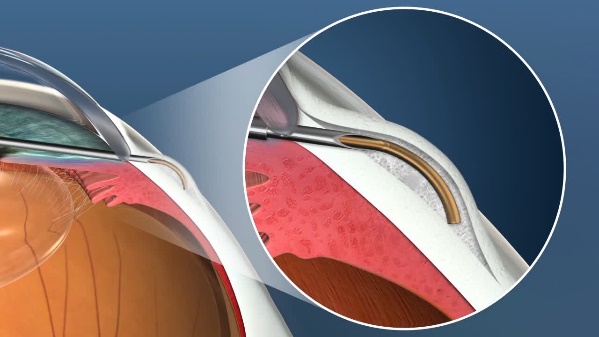
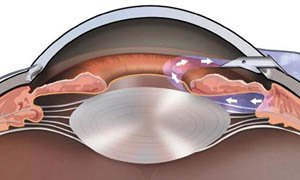
The XEN Gel Microstent is a very small glaucoma implant designed to reduce intraocular pressure in difficult to control glaucoma cases. It is placed using a fine delivery injector. It creates a channel that connects the anterior chamber to the subconjunctival space, allowing aqueous humor to flow into a small reservoir called a bleb. The fluid is then absorbed into the blood stream around the eye. The stent is designed to remain in the eye permanently.
Relative Size of the XEN Stent
Position of the XEN Stent in the Eye
The XEN stent can be placed in the eye alone or combined with cataract surgery. It is placed through a tiny incision in the cornea that is self-sealing. The recovery is rapid, and most patients can resume regular activities the next day.
The XEN is designed to reduce the risk of problems that are sometimes seen with larger, conventional glaucoma implants.
The XEN represents a major advance in glaucoma surgery because it provides the benefits of good reduction in intraocular pressure seen with larger shunts, with the safety profile seen with the smaller MIGS devices.
As with all glaucoma surgeries, the XEN stent may fail to control the eye pressure at some point after the surgery. If this occurs, additional surgery may be required.
The iStent Micro-Bypass glaucoma implant is the smallest of the MIGS devices. It is used for mild or moderate cases of glaucoma where the intraocular pressure is already adequately controlled with topical medications. The iStent can allow the patient to reduce or eliminate glaucoma eye drops.
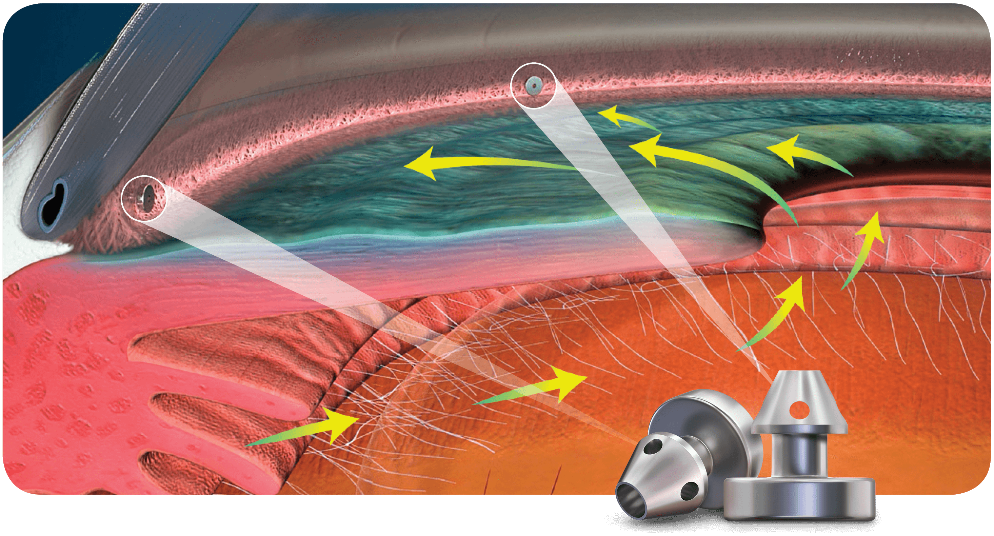
The iStent is always placed at the time of cataract surgery. The stent is placed in the trabecular meshwork to allow aqueous to flow more freely and leave the eye through its natural pathway. The iStent is delivered with an injector through the same self-sealing corneal incision used for the cataract surgery. Two individual stents are placed during the same procedure, in separate locations of the trabecular meshwork.
Relative Size of the iStent
Position of iStents in the Eye
Because the device is so small, there are fewer risks of problems associated with it compared to the large glaucoma implants. In addition, it does not add any additional recovery time to the cataract surgery. However, its small size limits the amount of IOP lowering that can be achieved, which is why it is reserved for glaucoma that is at an early stage.
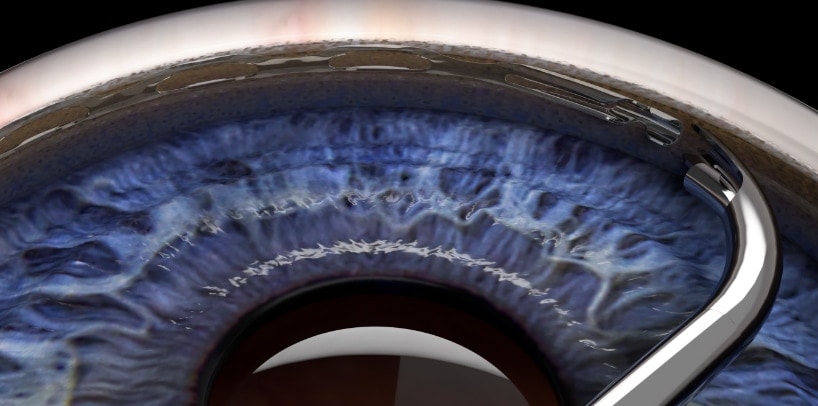
The Hydrus Microstent is a glaucoma implant that is part of the MIGS group of devices. It is used for mild or moderate cases of glaucoma where the intraocular pressure is already adequately controlled with topical medications. The Hydrus can allow the patient to reduce or eliminate glaucoma eye drops.
Relative Size of the Hydrus Stent
Placement of the Hydrus in the Eye
The Hydrus is always placed at the time of cataract surgery. The stent is placed in Schlemm’s canal to allow aqueous to more freely and leave the eye through its natural pathway. The Hydrus is placed with a special delivery device through the same self-sealing corneal incision used for the cataract surgery.
Because the device is so small, there are fewer risks of problems associated with it compared to the large glaucoma implants. In addition, it does not add any additional recovery time to the cataract surgery. However, its small size limits the amount of IOP lowering that can be achieved, which is why it is reserved for glaucoma that is at an early stage.
Glaucoma Drainage Implants are a group of procedures that are the conventional incisional surgeries for glaucoma. These surgeries are indicated for more advanced glaucomas, where the disease is more severe, and the eye pressure is much more difficult to control. Glaucoma drainage implants are often used for secondary glaucomas.
Glaucoma drainage implants are larger devices and require more manipulation to implant. The surgeries take longer to perform than the MIGS procedures, and there is a longer recovery period. However, they are necessary in cases where MIGS procedures will not work.
The risks of post-operative problems are increased with glaucoma drainage implant surgeries, in part, because the eye pressures are usually extremely high to start, and the eyes have more complex glaucoma problems.
The Ahmed Glaucoma Valve is a commonly used glaucoma implant. The device is composed of plastic and consists of a tube connected to a plate with a valve mechanism. The tube is inserted into the anterior chamber of the eye, and the plate is secured to the eye further back. The tube drains the aqueous fluid out of the eye into a reservoir above the plate. When fully healed, the patient does not feel or see the device in place.
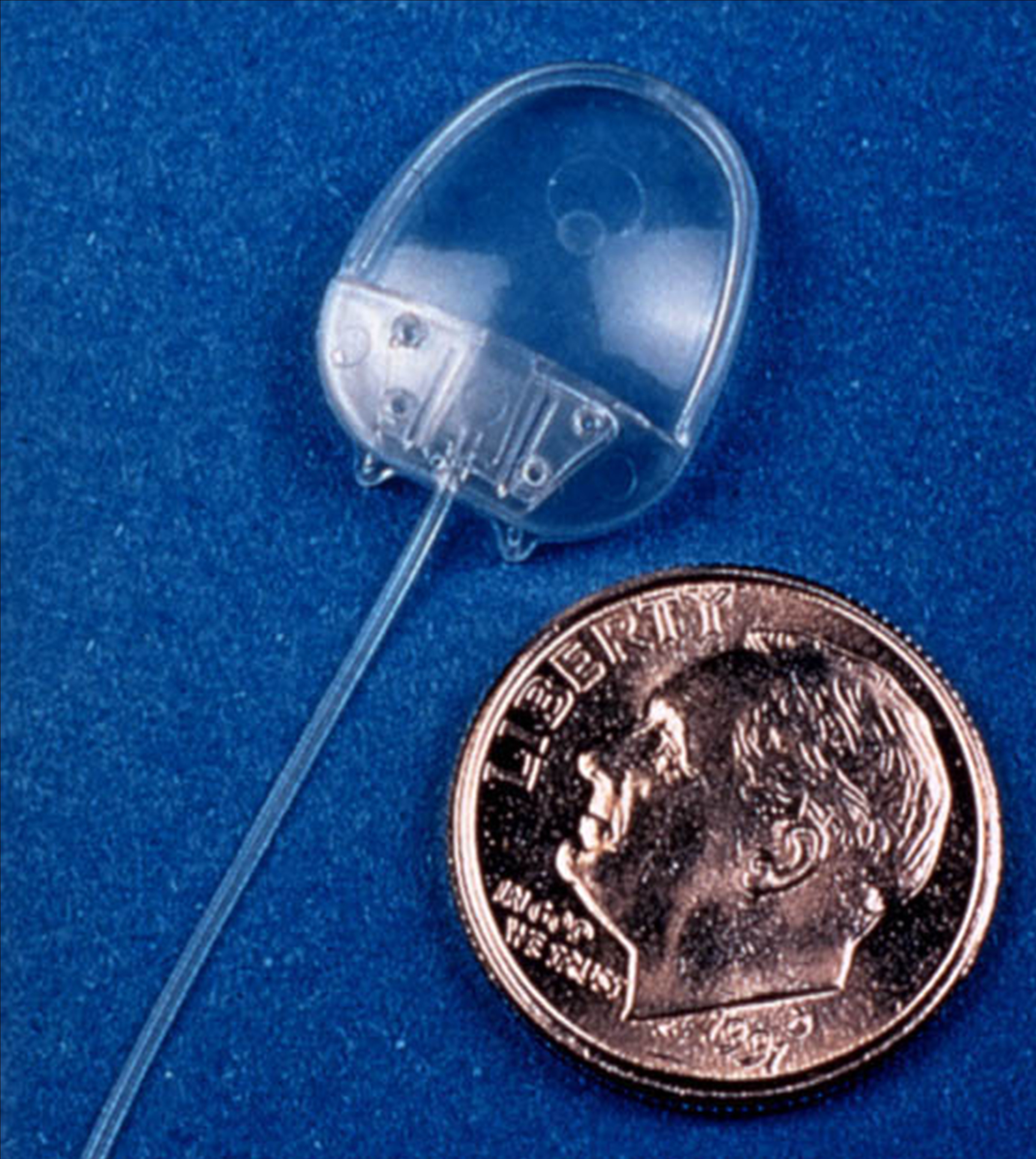
Relative size of the Ahmed Glaucoma Valve
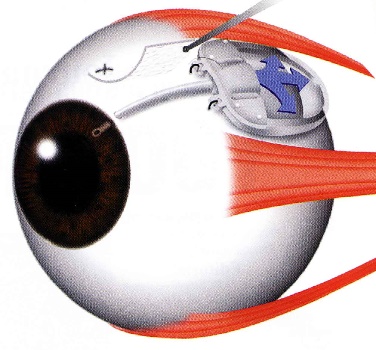
Position of the Ahmed Valve on the Eye
The surgery to place the Ahmed valve usually takes about 45 minutes to perform and is done under local anesthesia. The healing time can take up to a few weeks, but patients can resume most regular activities quickly.
The valve functions to lower the intraocular pressure immediately and is designed to work long-term. Because of the relatively large diameter of the tube, and the position of the plate, the valve is not at high risk for scarring. However, the eye pressure does not always end up as low with the Ahmed valve as with some other glaucoma devices.
The Ahmed valve is preferred when the goal is rapid lowering of intraocular pressure.
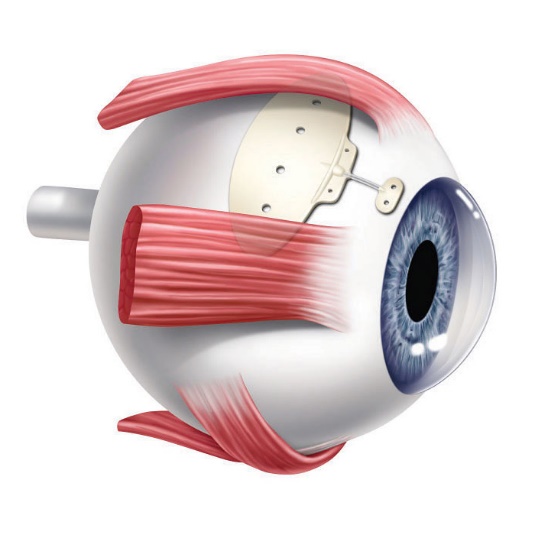
The Baerveldt Drainage Implant is the most reliable of all the glaucoma surgeries. It is very effective at achieving low intraocular pressure and is likely to function long-term. The device is composed of plastic and consists of a tube connected to a large plate, but with no valve mechanism. The tube is inserted into the anterior chamber of the eye, and the plate is secured to the eye further back. The tube drains the aqueous out of the eye into a reservoir above the plate. When fully healed, the patient does not feel or see the device in place.
Baerveldt Drainage Implant
Dr. Tesser performing Baerveldt Implant Surgery
The Baerveldt implant surgery takes longer to perform than other glaucoma surgery, and there is usually a longer healing time, up to several weeks, due to its larger size. There is often a delay in the lowering of the eye pressure because the non-valved tube of the device is intentionally tied off with a suture designed to dissolve very slowly. Because of the relatively large diameter of the tube, and the size and position of the plate, the shunt is not at high risk for scarring, and can achieve low eye pressures. The Baerveldt glaucoma implant is best suited for eyes requiring low final eye pressures, and in situations where the other glaucoma devices are likely to fail.
The Ex-Press Mini Shunt is a smaller glaucoma drainage implant device and the surgery, as its names implies, is quicker to perform. The Ex-Press Mini Shunt is a variation of a standard glaucoma operation procedure called a trabeculectomy, often called glaucoma filtration surgery.
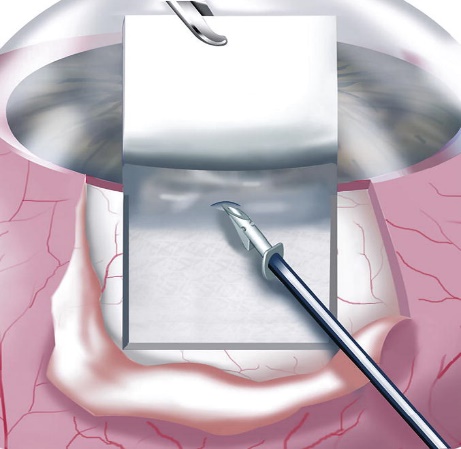
The Ex-Press shunt is made of stainless steel. It is a small stent that is placed under a flap of sclera and inserted into the anterior chamber. Aqueous humor fluid flows through the shunt out of the eye into a small reservoir called a bleb. The aqueous is then absorbed by the bleb into the blood circulation of the eye:
Ex-Press Shunt Implantation Under Scleral Flap
Drainage of aqueous humor through the Ex-Press Shunt
The Ex-Press shunt is designed to remain in the eye permanently. It can achieve very low intraocular pressures because the bleb that it creates is often very thin. However, because of its small size it can also stop working due to scar tissue. The Ex-Press Mini Shunt is preferred when the goal of the glaucoma surgery is to achieve the lowest possible pressure.
Cataract and Glaucoma Surgery are often performed together as combined procedures. This is because there is significant overlap between cataracts and glaucoma.
The lens of the eye, because of its position and size, can have significant effects on the fluid flow in the eye, causing the eye pressure to increase. Some glaucoma conditions, such as angle closure glaucoma, are the result of an enlarging cataract.
Some conditions, such as steroid use or diabetes, can cause both cataracts and glaucoma.
Some secondary glaucomas, such as exfoliation glaucoma, are associated with both complex glaucoma and cataracts, each of which more difficult to treat.
As a result, in these and other situations, it is often more efficient to combine the glaucoma and cataract surgeries. The combined surgery can simultaneously achieve both improved vision and a lowering of the eye pressure. In addition, it is more convenient for the patient to have both types of surgery at the same time.
In cases where the glaucoma is mild, and there is a coexisting cataract, combining cataract surgery with a MIGS procedure can reduce or eliminate the number of glaucoma drops that need to be used. In more severe glaucomas, the cataract surgery can be combined with a glaucoma drainage implant.
In certain situations, however, it is best to perform sequential procedures, at different times. This often depends on the relative complexity and severity the cataract or the glaucoma. Either the glaucoma surgery or the cataract surgery can be performed first, followed by the second type of procedure. The time between the procedures can be anywhere from weeks to months, in order to allow the eye to recover form the first procedure.
Make an Appointment