Glaucoma is an eye disease in which the eye pressure (intraocular pressure) is too high for the eye, causing damage to the optic nerve, resulting in loss of vision.
Proper glaucoma management involves examining and monitoring all parts of the eye that are related to the pressure and optic nerve function. This is accomplished by employing a variety of testing modalities. Not every test needs to be performed at each examination. But it is important that the appropriate tests are performed when needed.
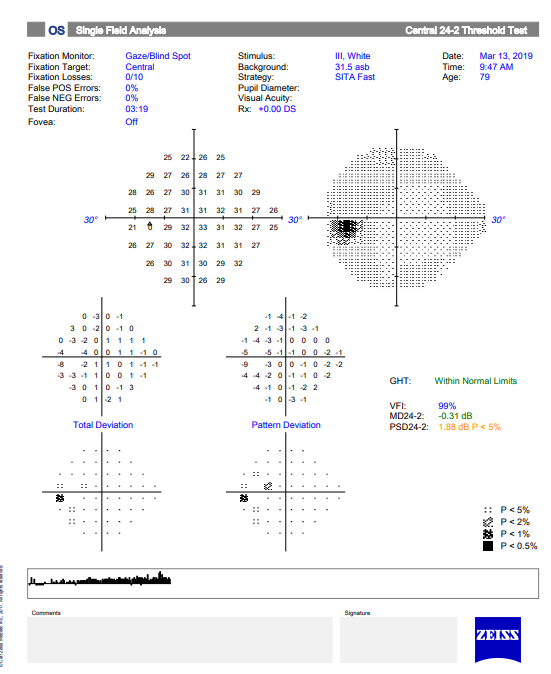
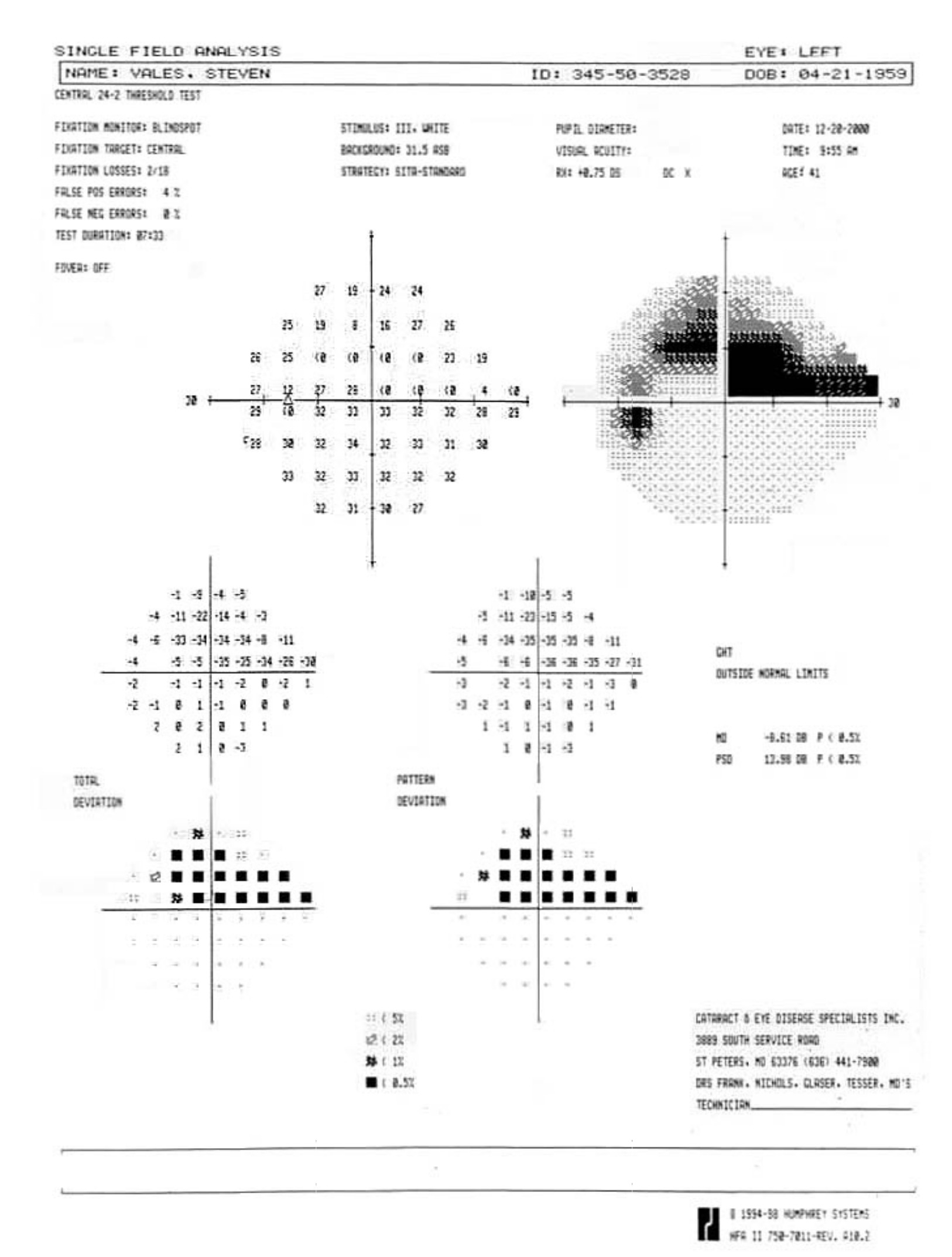
Visual Field Testing is an essential component of glaucoma diagnosis and management.
The visual field refers to the entire area that an eye sees, from the outside (peripheral) vision to the very central vision. When the optic nerve is damaged in glaucoma, this results in loss of parts or all the visual field. The lost area of visual field is referred to as a blind spot or scotoma. The main goals of glaucoma therapy are to prevent the development of visual field loss, and if visual field loss has already developed, to prevent further progression.
Often, the visual field loss is not noticeable by the patient until it is advanced, at which point it can interfere with regular activities such as driving:
Normal Visual Field
Advanced Visual Field Loss
Severe Visual Field Loss
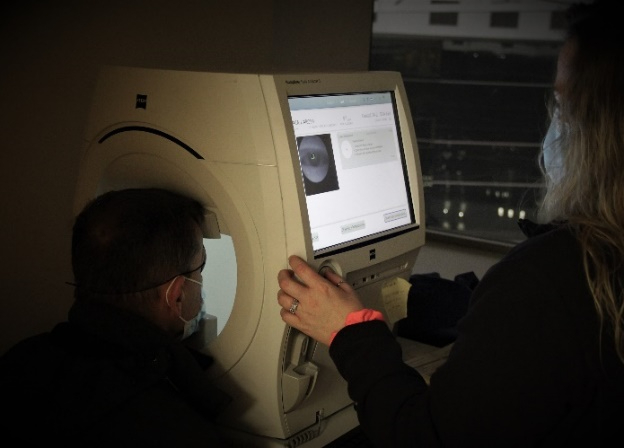
The device used to test the visual field is called a perimeter, and visual field testing is also called perimetry. There are several types of perimeters available, and each has different types of test patterns and stimuli. The testing involves the patient looking into the perimeter bowl, while focusing (fixating) on a central point. Different types of target light (the stimulus) are then projected at random points in the perimeter and the patient clicks a button when a target light is seen. The visual field is then mapped out and displayed.
Visual field testing is a simple test and usually takes just a few minutes to perform on an eye. Because of the central role that visual field testing plays in glaucoma management, it is important that patients undergo the appropriate type of testing at regular intervals, usually every few months, in order to ensure accuracy.
The two main visual field tests that we perform on patients are Standard Automated Perimetry (SAP) and Frequency-Doubling Perimetry (FDP). SAP functions better to monitor disease progression and FDP is more useful for early disease detection.
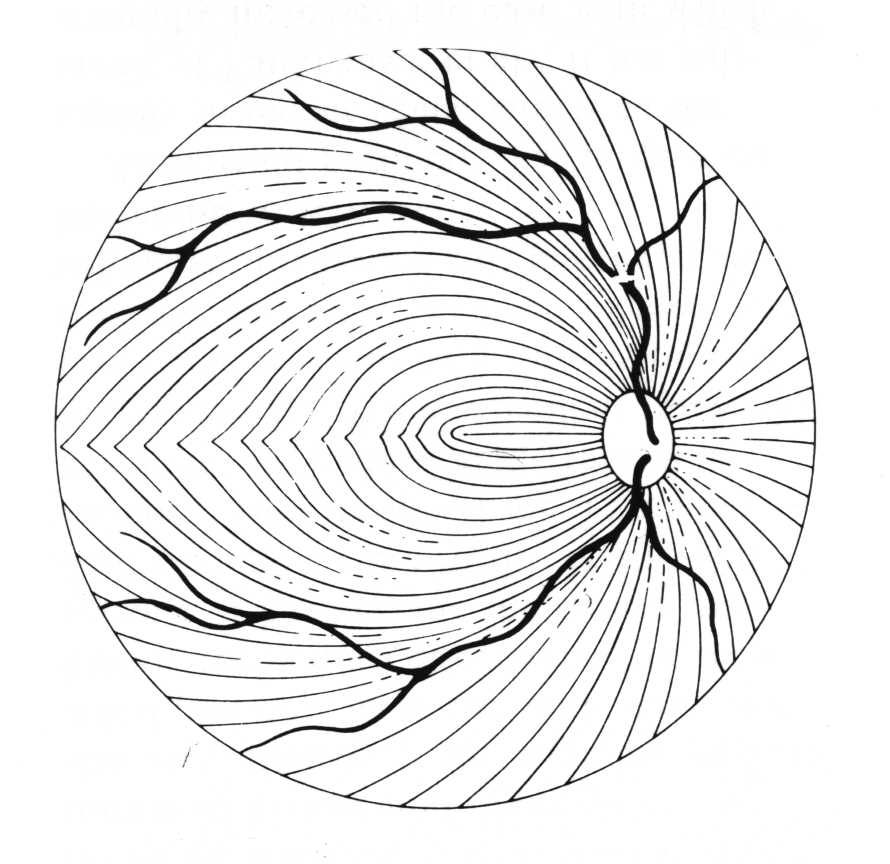
Because of the specific way the optic nerve and nerve fiber layer are damaged in glaucoma, the visual field loss that develops often appears in certain patterns. The nerve fiber layer extends across the retina in a curved pattern, so when it is damaged, the loss of vision follows that same pattern. These are usually called arcuate defects (since they are arc shaped).
Nerve Fiber Layer
Nerve Fiber Layer Damage
Arcuate Visual Field Loss
[Remember that the eye inverts an incoming image, so damage to the inferior (lower) nerve fiber layer results in superior (upper) visual field loss.]
In early glaucoma, the arcuate defects are small, and away from the central vision, so they might not be noticeable or symptomatic. If glaucoma worsens, the arcuate defects can extend from the peripheral to the central vision, at which point they start to affect how a patient sees. By the time a patient notices the visual field loss, the disease is considered advanced or severe.
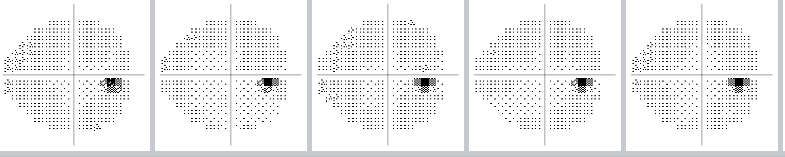
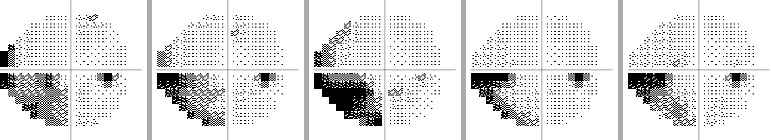
The visual field can be monitored over time to see if there is progression of glaucoma, or if the disease has stabilized as a result of treatment:
Example of a normal visual field over time
(The small dark spot is the eye’s "natural" blind spot.)
Example of a stabilized visual field over time
Example of progression of visual field loss over time
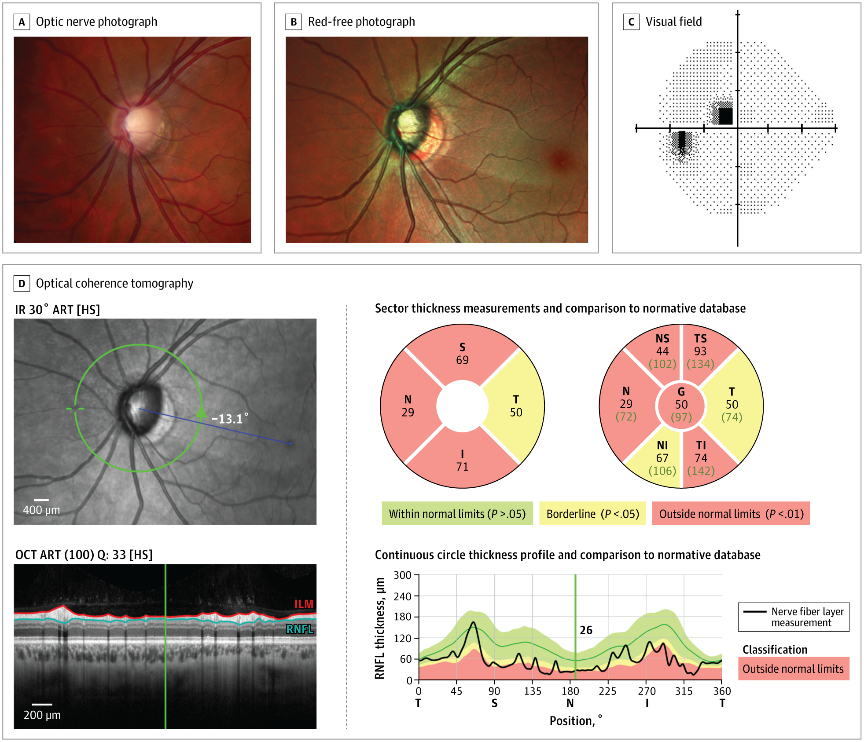
Optic Nerve Analysis is a central part of glaucoma diagnosis. Because the optic nerve is the site of injury in glaucoma, decisions about treatment are made based upon the degree of damage to the nerve.
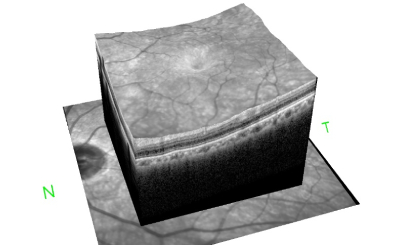
The optic nerve head is the part of the optic nerve that is susceptible to injury from elevated intraocular pressure. The optic nerve head can analyzed in three-dimensions by optical coherence tomography or imaged by fundus photography.
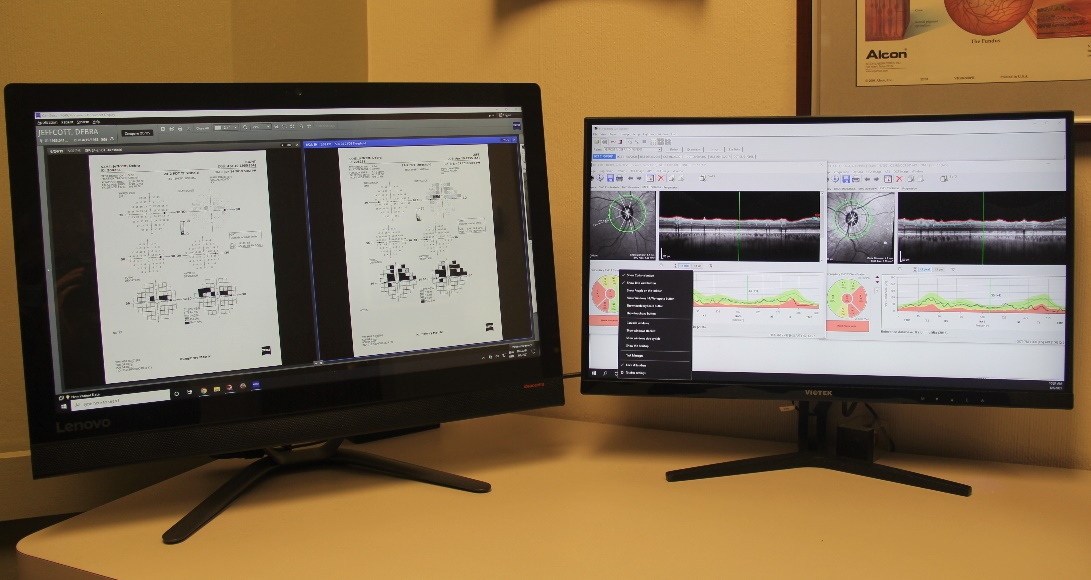
Optical Coherence Tomography
Fundus Photography
Each type of optic nerve analysis gives a different type of information Optical coherence tomography creates a 3-D image of the optic nerve head which can be monitored over time to see if there is are any changes in the nerve structure. . Fundus photography documents the appearance of the nerve in real color and allows for comparison with other examinations. As is the case for visual field testing, optic nerve analysis needs to be performed at regular intervals to determine if the glaucoma therapy is effective.
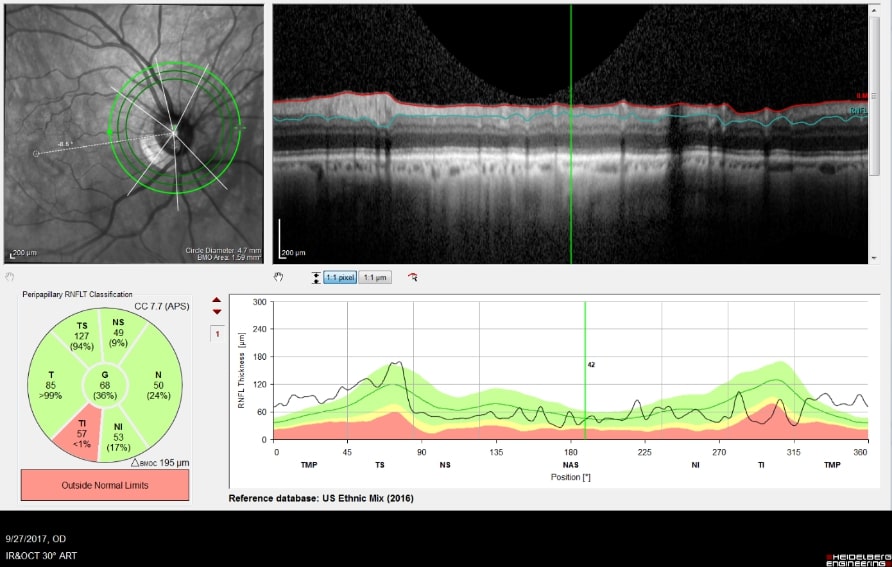
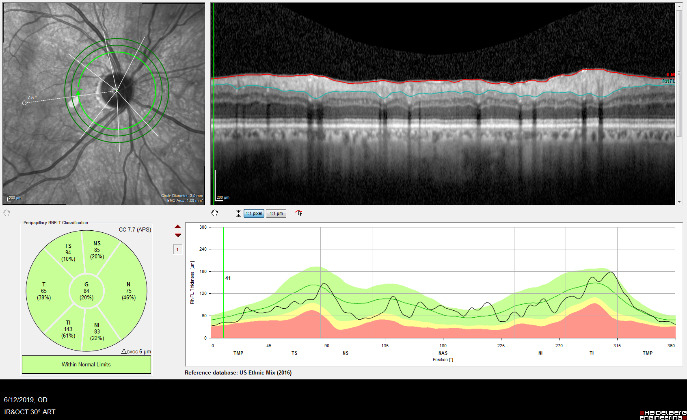
Optical Coherence Tomography (OCT) is an advanced imaging technology that has revolutionized the diagnosis and management of eye disease, especially glaucoma and retinal disease. OCT is a non-invasive method of imaging structures in the eye at an extremely high, microscopic resolution.
OCT uses infrared light to create cross-sectional, three-dimensional images of the tissues in the eye. As is the case for laser treatments, the eye is particularly amenable to imaging with OCT because the eye is optically transparent.
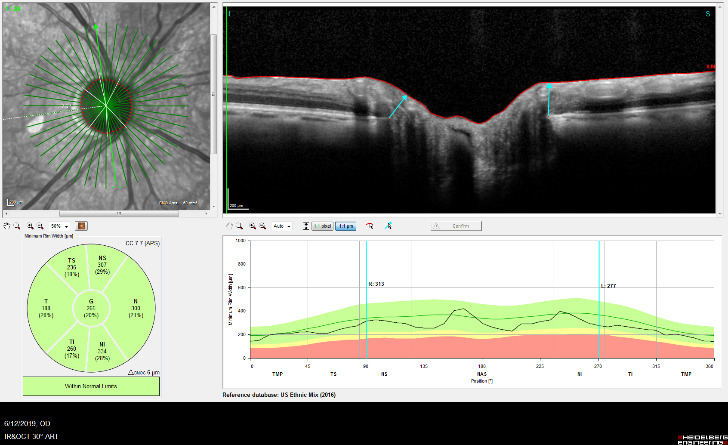
OCT Imaging of the Nerve Fiber Layer
OCT Image of the Retina
OCT is used in glaucoma to image the optic nerve and the nerve fiber layer in order to determine if there is damage from increased eye pressure. Because the resolution of OCT is so high, it can detect fine changes to the shape of optic nerve. Thinning of the nerve fiber layer is a sign that glaucoma is worsening and that the eye pressure is too high.
OCT Imaging of a Normal Optic Nerve
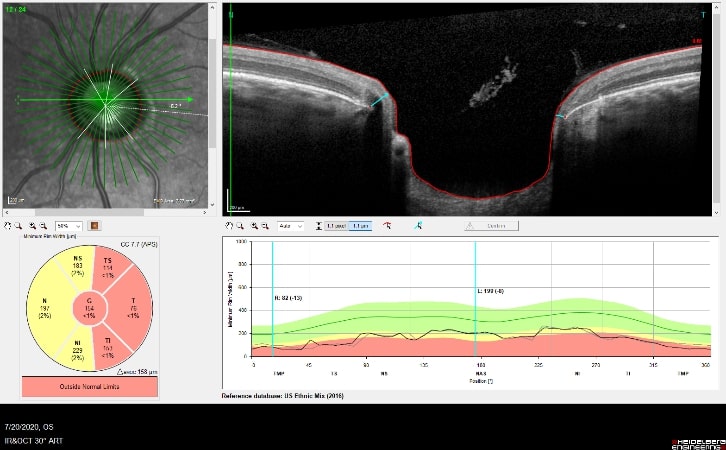
OCT Imaging showing a
Cupped Optic Nerve
Structural changes to the optic nerve or nerve fiber layer usually precede visual field loss. In many cases, 50% of the optic nerve can be damaged before visual field loss develops. As a result, OCT is a critical tool for diagnosing glaucoma at its earliest stages.
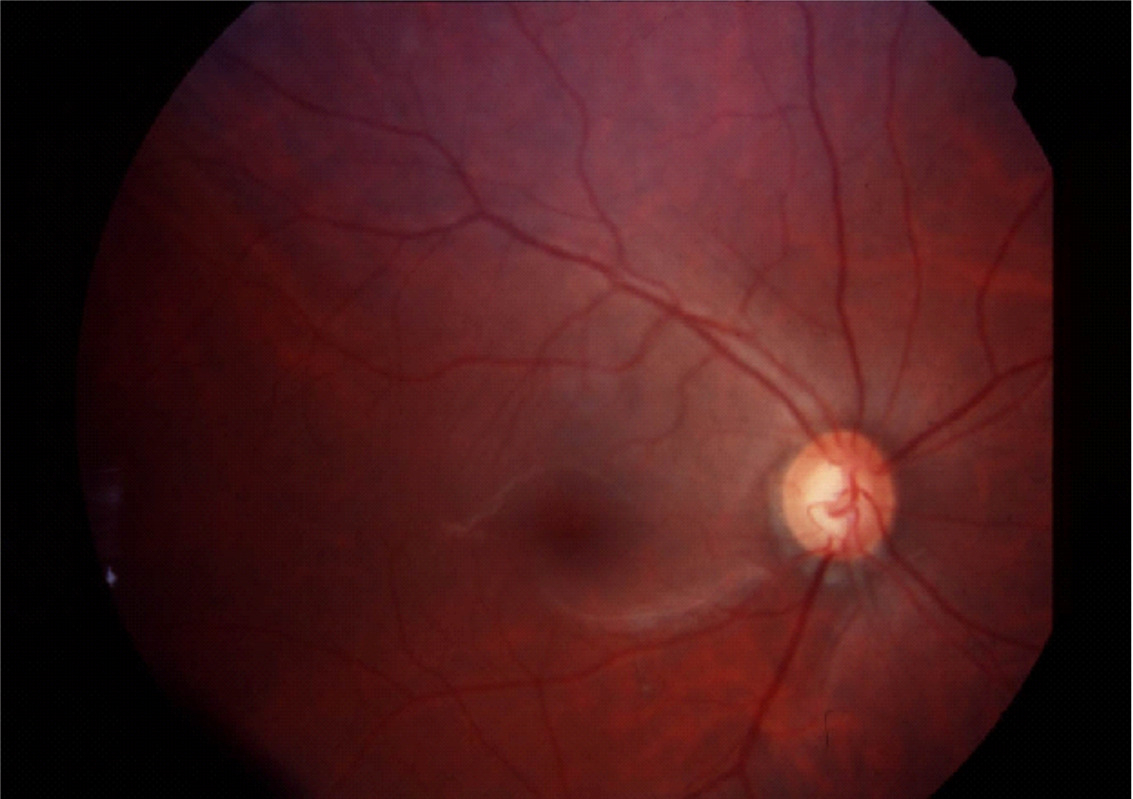
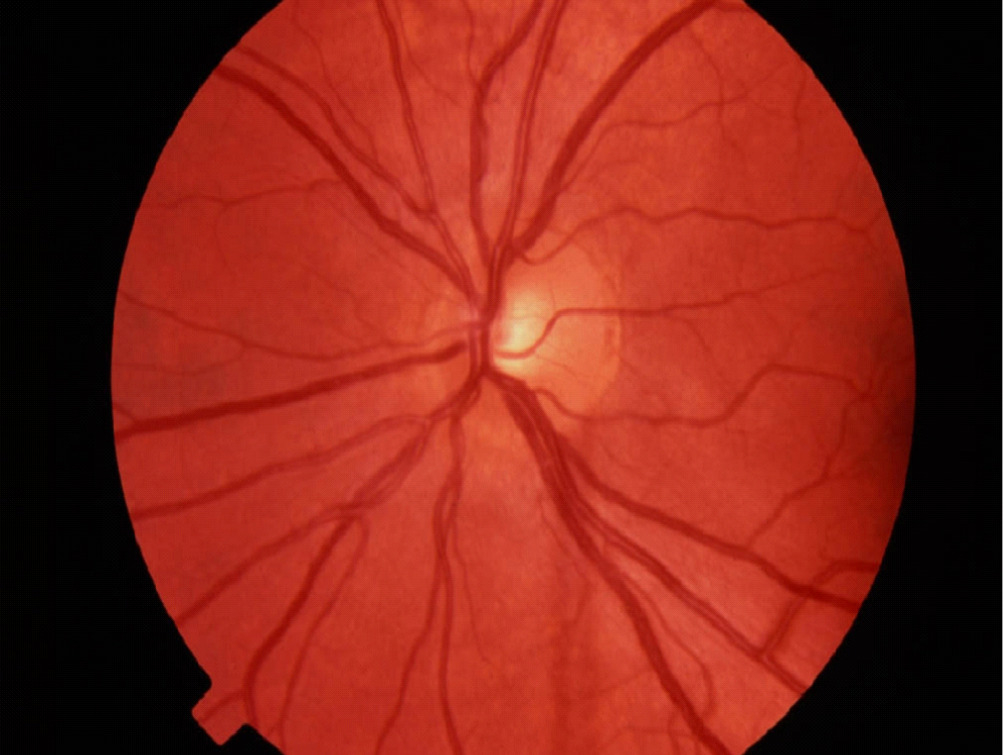
Fundus photography records digital photographic images of the back of the eye (the fundus). Specific parts of the fundus can be photographed such as the optic nerve and macula. Fundus photography compliments OCT in that it provides true color images of the different structures.
Normal Optic Nerve
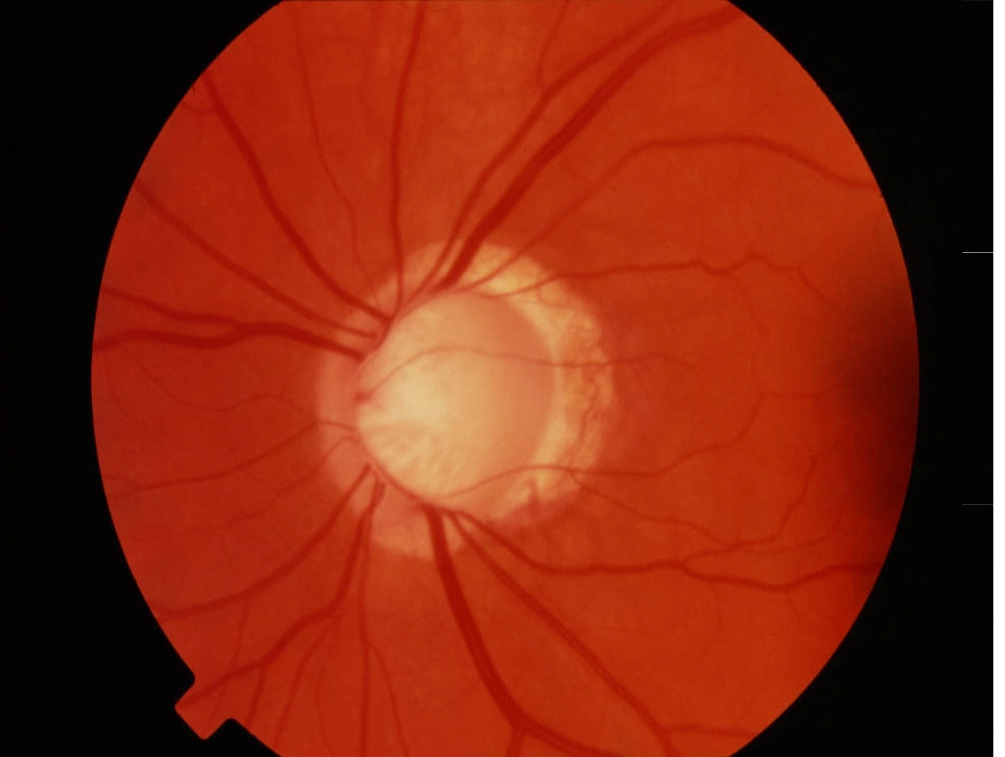
Glaucomatous Cupping
Fundus photography allows documentation of changes to the optic nerve that occur glaucoma including cupping, disc hemorrhages, atrophy, and loss of the nerve fiber layer. Certain filters can be used to enhance the visualization the nerve fiber layer.
An example of an optic nerve with glaucoma damage imaged with both fundus photography and OCT and compared to the visual field in order to demonstrate the strucure-function relationship.
The lower half of the optc nerve has early damage, and this correlates with the small superior scotoma seen on the visual field test.
Intraocular Pressure (IOP) measurement is performed at every eye examination. Because all glaucoma treatments are designed to lower intraocular pressure, it is essential that accurate IOP measurements are made to determine effectiveness of treatment.
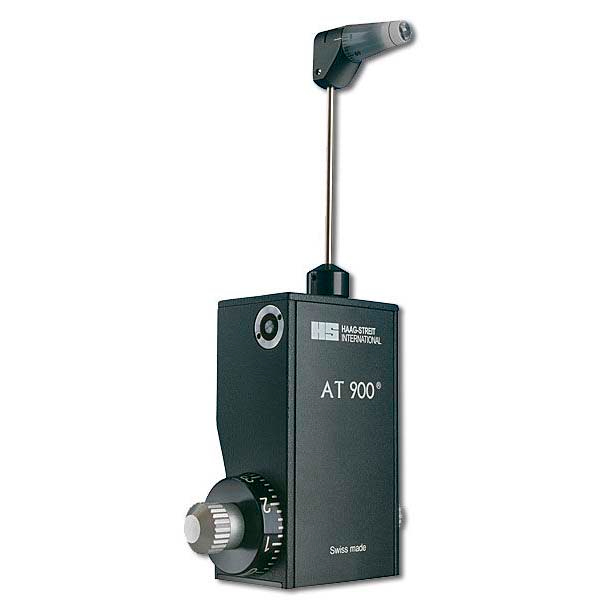
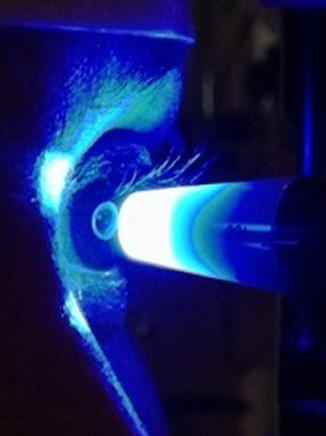
There are many different methods for measuring eye pressure. The most precise and reliable is Goldmann Applanation Tonometry (GAT, or simply applanation) . Other, less reliable methods include Non-Contact Tonometry (NCT, which is also referred to as the “air-puff” test) and the Tono-Pen (which is an electronic measurement).
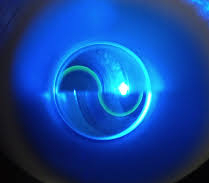
GAT determines the IOP by using a tonometer tip to physically contact the eye and flatten (applanate) the central cornea. The in order to visualize the applanation, an orange dye (fluorescein) is placed on the eye to color the tear film, along with a numbing drop. The tonometer tip is then illuminated with a blue light causing the dye to fluoresce. When the cornea is flattened with a pressure that equals the pressure in the eye, two semicircle rings line up as seen through the slit-lamp. The tension is then read off a dial on the tonometer base and converted to mm Hg (millimeters of Mercury, the units of pressure).
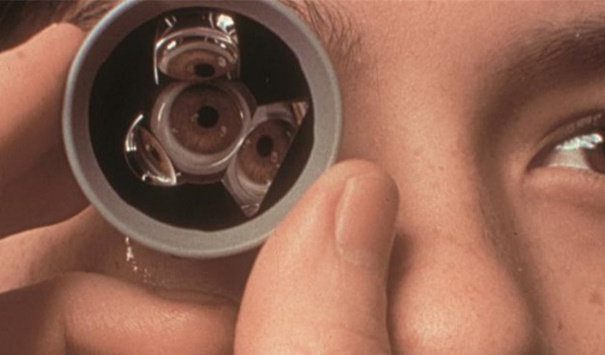
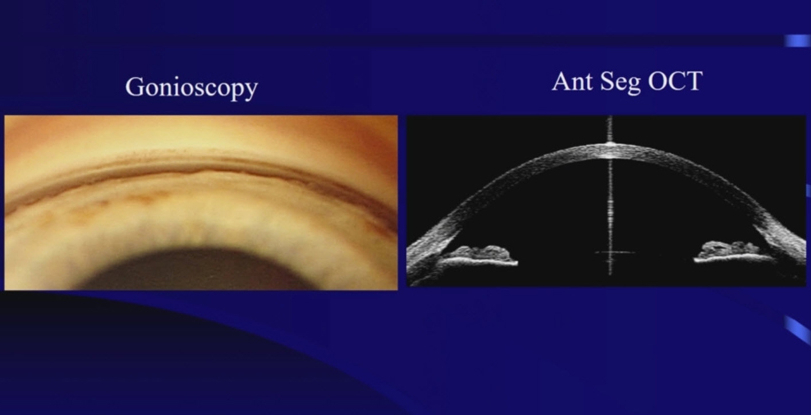
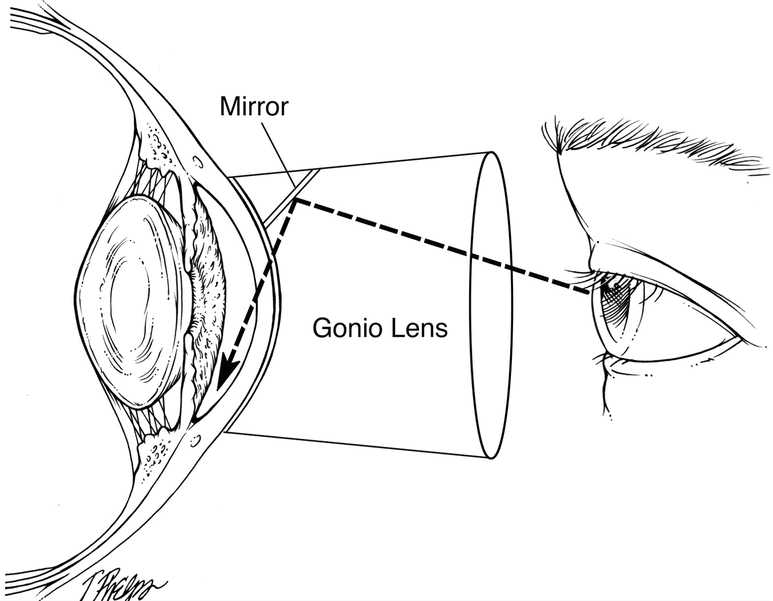
Gonioscopy examines the outflow angle where the aqueous humor drains from the eye. Gonioscopy determines whether the glaucoma is of the open angle or closed angle type.
Because of the structure of the eye, the outflow angle cannot be seen directly. A special lens, called a gonioprism is required to see the angle structures indirectly using reflected light. Because the angle is the site of the eye where Selective Laser Trabeculoplasty is performed, a gonioprism is also used for the laser treatment.
Optical Coherence Topography can also be used to analyze the anatomy of the outflow angle, in a three-dimensional view.
Pachymetry is a test that is performed to determine the central thickness of the cornea. Thinner corneas are associated with increased risk of glaucoma and thicker corneas are associated with a lower risk of glaucoma. The cornea itself is not involved in the development of glaucoma, but rather the thickness serves as a marker for relative risk.
Corneal pachymetry measurements are very quick to perform, using a hand-held electronic ultrasound device.
Make an Appointment